A Sample Of Notes From Medical Virology // I Keep The Margins Empty So That I Have Space To Add In Relevant




A sample of notes from Medical Virology // I keep the margins empty so that I have space to add in relevant additional material from extra reading
More Posts from T-b-a-blr-blog and Others
Clostridium tetani
Gram+, anaerobe, spore forming, motile, rod.
Neurotoxin: Tetanus Toxin blocks glycine and GABA and produces a SPASTIC PARALYSIS.
TETANUS
Opisthotonus

Risus Sardonicus

Severe mucle spasm


study tip request: studying on public transport (or sth related like how to know what to record when you record yourself saying notes so that you can listen to them on public transport)
Best Way to Make Study Recordings for Yourself
Testing yourself is the most effective way to learn a topic, so this one is fairly straightforward. For recording:
Formulate an examination style question, and run through the answer in your head, organising your thoughts.
Then record the question, and mouth silently the answer fluently (reason being that just thinking in your head may result in too little or too much silence.
Leave a few extra seconds of silence for thinking time (~3-5 seconds).
Answer the question aloud in the recording (I’d suggest a brief one)
Rinse and repeat until you have enough to last you the whole commute.
Hope that helps! For more tips on how to spend time on commutes, check out my post on Staying Productive No Matter How Much Time You Have :)


30 . 06 . 2017 Microbiology notes !!! Yesterday I took my physics final exam and it went great: I got a 27/30, which is way more than what I expected as Physics is one of my worst subjects. My next exam, microbiology, is in four days and I’m starting to feel a bit anxious about it as it’s a pretty tough exam but I’ll try to do my best !
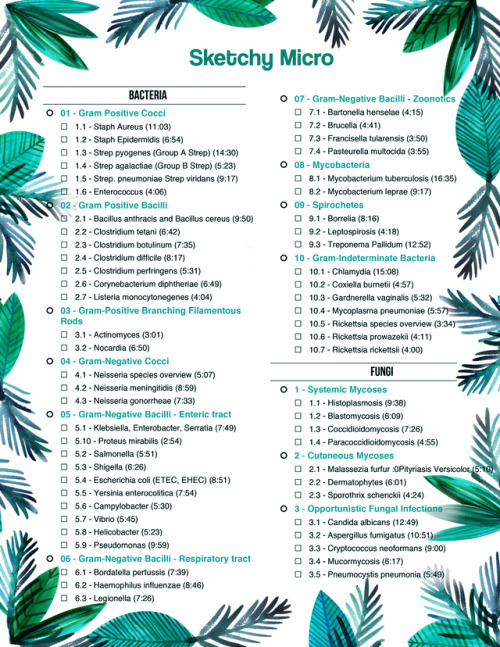
Sketchy Micro To Do List:
• 01 - Gram Positive Cocci o 1.1 - Staph Aureus (11:03) o 1.2 - Staph Epidermidis (6:54) o 1.3 - Strep pyogenes (Group A Strep) (14:30) o 1.4 - Strep agalactiae (Group B Strep) (5:23) o 1.5 - Strep. pneumoniae Strep viridans (9:17) o 1.6 - Enterococcus (4:06) • 02 - Gram Positive Bacilli o 2.1 - Bacillus anthracis and Bacillus cereus (9:50) o 2.2 - Clostridium tetani (6:42) o 2.3 - Clostridium botulinum (7:35) o 2.4 - Clostridium difficile (8:17) o 2.5 - Clostridium perfringens (5:31) o 2.6 - Corynebacterium diphtheriae (6:49) o 2.7 - Listeria monocytonegenes (4:04) • 03 - Gram-Positive Branching Filamentous Rods o 3.1 - Actinomyces (3:01) o 3.2 - Nocardia (6:50) • 04 - Gram-Negative Cocci o 4.1 - Neisseria species overview (5:07) o 4.2 - Neisseria meningitidis (8:59) o 4.3 - Neisseria gonorrheae (7:33) • 05 - Gram-Negative Bacilli - Enteric tract o 5.1 - Klebsiella, Enterobacter, Serratia (7:49) o 5.10 - Proteus mirabilis (2:54) o 5.2 - Salmonella (5:51) o 5.3 - Shigella (6:26) o 5.4 - Escherichia coli (ETEC, EHEC) (8:51) o 5.5 - Yersinia enterocolitica (7:54) o 5.6 - Campylobacter (5:30) o 5.7 - Vibrio (5:45) o 5.8 - Helicobacter (5:23) o 5.9 - Pseudomonas (9:59) • 06 - Gram-Negative Bacilli - Respiratory tract o 6.1 - Bordatella pertussis (7:39) o 6.2 - Haemophilus influenzae (8:46) o 6.3 - Legionella (7:26)
• 07 - Gram-Negative Bacilli - Zoonotics o 7.1 - Bartonella henselae (4:15) o 7.2 - Brucella (4:41) o 7.3 - Francisella tularensis (3:50) o 7.4 - Pasteurella multocida (3:55) • 08 - Mycobacteria o 8.1 - Mycobacterium tuberculosis (16:35) o 8.2 - Mycobacterium leprae (9:17) • 09 - Spirochetes o 9.1 - Borrelia (8:16) o 9.2 - Leptospirosis (4:18) o 9.3 - Treponema Pallidum (12:52) • 10 - Gram-Indeterminate Bacteria o 10.1 - Chlamydia (15:08) o 10.2 - Coxiella burnetii (4:57) o 10.3 - Gardnerella vaginalis (5:32) o 10.4 - Mycoplasma pneumoniae (5:57) o 10.5 - Rickettsia species overview (3:34) o 10.6 - Rickettsia prowazekii (4:11) o 10.7 - Rickettsia rickettsii (4:00) • Fungi • 1 - Systemic Mycoses o 1.1 - Histoplasmosis (9:38) o 1.2 - Blastomycosis (6:09) o 1.3 - Coccidioidomycosis (7:26) o 1.4 - Paracoccidioidomycosis (4:55) • 2 - Cutaneous Mycoses o 2.1 - Malassezia furfur :0Pityriasis Versicolor (5:10) o 2.2 - Dermatophytes (6:01) o 2.3 - Sporothrix schenckii (4:24) • 3 - Opportunistic Fungal Infections o 3.1 - Candida albicans (12:49) o 3.2 - Aspergillus fumigatus (10:51) o 3.3 - Cryptococcus neoformans (9:00) o 3.4 - Mucormycosis (6:17) o 3.5 - Pneumocystis pneumonia (5:49)
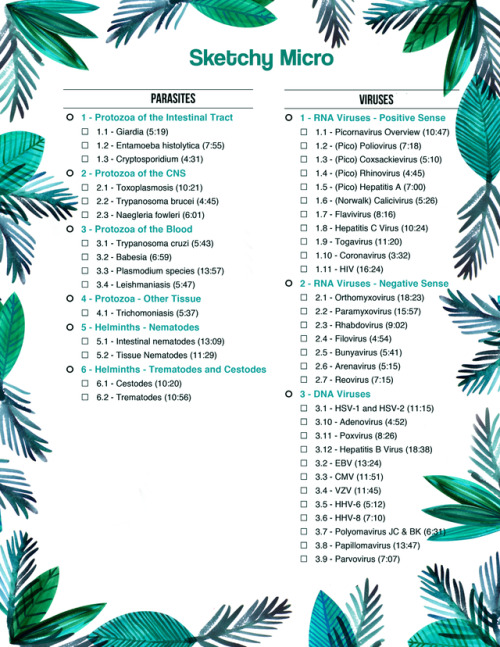
• Parasites • 1 - Protozoa of the Intestinal Tract o 1.1 - Giardia (5:19) o 1.2 - Entamoeba histolytica (7:55) o 1.3 - Cryptosporidium (4:31) • 2 - Protozoa of the CNS o 2.1 - Toxoplasmosis (10:21) o 2.2 - Trypanosoma brucei (4:45) o 2.3 - Naegleria fowleri (6:01) • 3 - Protozoa of the Blood o 3.1 - Trypanosoma cruzi (5:43) o 3.2 - Babesia (6:59) o 3.3 - Plasmodium species (13:57) o 3.4 - Leishmaniasis (5:47) • 4 - Protozoa - Other Tissue o 4.1 - Trichomoniasis (5:37) • 5 - Helminths - Nematodes o 5.1 - Intestinal nematodes (13:09) o 5.2 - Tissue Nematodes (11:29) • 6 - Helminths - Trematodes and Cestodes o 6.1 - Cestodes (10:20) o 6.2 - Trematodes (10:56)
• Viruses • 1 - RNA Viruses - Positive Sense o 1.1 - Picornavirus Overview (10:47) o 1.2 - (Pico) Poliovirus (7:18) o 1.3 - (Pico) Coxsackievirus (5:10) o 1.4 - (Pico) Rhinovirus (4:45) o 1.5 - (Pico) Hepatitis A (7:00) o 1.6 - (Norwalk) Calicivirus (5:26) o 1.7 - Flavivirus (8:16) o 1.8 - Hepatitis C Virus (10:24) o 1.9 - Togavirus (11:20) o 1.10 - Coronavirus (3:32) o 1.11 - HIV (16:24) • 2 - RNA Viruses - Negative Sense o 2.1 - Orthomyxovirus (18:23) o 2.2 - Paramyxovirus (15:57) o 2.3 - Rhabdovirus (9:02) o 2.4 - Filovirus (4:54) o 2.5 - Bunyavirus (5:41) o 2.6 - Arenavirus (5:15) o 2.7 - Reovirus (7:15) • 3 - DNA Viruses o 3.1 - HSV-1 and HSV-2 (11:15) o 3.10 - Adenovirus (4:52) o 3.11 - Poxvirus (8:26) o 3.12 - Hepatitis B Virus (18:38) o 3.2 - EBV (13:24) o 3.3 - CMV (11:51) o 3.4 - VZV (11:45) o 3.5 - HHV-6 (5:12) o 3.6 - HHV-8 (7:10) o 3.7 - Polyomavirus JC & BK (6:31) o 3.8 - Papillomavirus (13:47) o 3.9 - Parvovirus (7:07)


Hope it helps @shreeparn :)


18/1/18 - Recent virology notes! Ignore the headings, I bought some new brush pens and I’m still getting used to them..
Gram Negative Aerobic Rods Mnemonic
MICROBIOLOGY MNEMONIC
BRUno, FRANCISco & COnstantine are BORing PSEUDO LEGIONnaires
Brucella sp
Francisella tularensis
Coxiella burnetti
Bortedella pertusis
Pseudomona aeuroginosa
Legionella pneumophila
Antimicrobial Agents - Inhibition of DNA and Protein Synthesis
Bacterial chromosome replication

DNA replication

Bacterial Topoisomerases
maintain DNA in appropriate state of supercoiling
cut and reseal DNA
DNA gyrase (topoisomerase II) introduces negative supercoils
Topoisomerase IV decatenates circular chromosomes
these are the targets of the quinolone antibacterial agents
Quinolones
bind to bacterial DNA gyrase and topoisomerase IV after DNA strand breakage
prevent resealing of DNA
disrupt DNA replication and repair
bactericidal (kill bacteria)
Fluoroquinolone is particularly useful against
Gram +ves: Staphylococcus aureus, streptococci
Gram -ves: Enterobacteriacea; Pseudomonas aeruginosa
Anaerobes: e.g. Bacteroides fragilis
many applications e.g. UTIs, prostatitis, gastroenteritis, STIs
Adverse effects
Relatively well tolerated
GI upset in ~ 5% of patients
allergic reactions (rash, photosensitivity) in 1 - 2% of patients

Inhibition of Bacterial Protein Synthesis
Macrolides
in 1952: Erythromycin was isolated as the first macrolide (Streptomyces erythreus)
Newer macrolides: clarithromycin, azithromycin
Structurally they consist of a lactone ring (14- to 16-membered) + two attached deoxy sugars
Mode of action
bind reversibly to bacterial 50S ribosomal subunit
causes growing peptide chain to dissociate from ribosome → inhibiting protein synthesis
bacteriostatic (stops reproduction)

Macrolides’ spectrum of activity
good antistaphylococcal and antistreptococcal activity
treatment of respiratory & soft tissue infections and sensitive intracellular pathogens • e.g. Chlamydia, Legionella
Adverse effects
Generally well tolerated
nausea
vomiting
diarrhoea
rash
Aminoglycosides
large family of antibiotics produced by various species of Streptomyces (“mycin”) and Micromonospora (“micin”)
include: streptomycin, neomycin, kanamycin, gentamicins, tobramycin
Structure = linked ring system composed of aminosugars and an aminosubstituted cyclic polyalcohol
Mode of action of aminoglycosides
Bind irreversibly to 30S ribosomal subunit
disrupt elongation of nascent peptide chain
translational inaccuracy → defective proteins
bactericidal

Spectrum of activity
broad spectrum; mainly aerobic G-ve bacilli (e.g. P. aeruginosa)
used to treat serious nosocomial infections (hospital acquired infections)
First TB antibiotic
Used for cystic fibrosis
Adverse effects
all aminoglycosides have low Therapeutic Index (only a small amount needed to become toxic)
renal damage, ototoxicity, loss of balance, nausea
-
 alux-ulkan liked this · 5 years ago
alux-ulkan liked this · 5 years ago -
 lux321 liked this · 5 years ago
lux321 liked this · 5 years ago -
 piggy-power liked this · 6 years ago
piggy-power liked this · 6 years ago -
 sweetmemoriies liked this · 6 years ago
sweetmemoriies liked this · 6 years ago -
 bolioptics liked this · 6 years ago
bolioptics liked this · 6 years ago -
 inspiredbylukas liked this · 6 years ago
inspiredbylukas liked this · 6 years ago -
 wanttoshine-a liked this · 6 years ago
wanttoshine-a liked this · 6 years ago -
 viiirology reblogged this · 6 years ago
viiirology reblogged this · 6 years ago -
 tutaina liked this · 6 years ago
tutaina liked this · 6 years ago -
 notartemisa reblogged this · 6 years ago
notartemisa reblogged this · 6 years ago -
 medmood liked this · 6 years ago
medmood liked this · 6 years ago -
 lida1122 liked this · 6 years ago
lida1122 liked this · 6 years ago -
 niangaobunian liked this · 6 years ago
niangaobunian liked this · 6 years ago -
 tajomstvo-7 reblogged this · 6 years ago
tajomstvo-7 reblogged this · 6 years ago -
 takichita reblogged this · 6 years ago
takichita reblogged this · 6 years ago -
 adelinestudiess liked this · 6 years ago
adelinestudiess liked this · 6 years ago -
 sakuraberyl liked this · 6 years ago
sakuraberyl liked this · 6 years ago -
 dignifiedcustomer liked this · 6 years ago
dignifiedcustomer liked this · 6 years ago -
 a-rame reblogged this · 6 years ago
a-rame reblogged this · 6 years ago -
 kin-study reblogged this · 6 years ago
kin-study reblogged this · 6 years ago -
 cielstudies reblogged this · 6 years ago
cielstudies reblogged this · 6 years ago -
 oui-oui-madame-baguette liked this · 6 years ago
oui-oui-madame-baguette liked this · 6 years ago -
 medizinstudentin-blog reblogged this · 6 years ago
medizinstudentin-blog reblogged this · 6 years ago -
 rainyhairdoeagleneck-blog liked this · 6 years ago
rainyhairdoeagleneck-blog liked this · 6 years ago -
 laviebohemefille liked this · 6 years ago
laviebohemefille liked this · 6 years ago -
 rocksolid10notcm liked this · 6 years ago
rocksolid10notcm liked this · 6 years ago -
 solo-davanti-allimmenso-mare liked this · 6 years ago
solo-davanti-allimmenso-mare liked this · 6 years ago -
 leainrumaenien liked this · 6 years ago
leainrumaenien liked this · 6 years ago -
 medizinstudentin-blog reblogged this · 6 years ago
medizinstudentin-blog reblogged this · 6 years ago -
 eliena1234 liked this · 6 years ago
eliena1234 liked this · 6 years ago -
 orangeblossomstudies reblogged this · 6 years ago
orangeblossomstudies reblogged this · 6 years ago -
 orangeblossomstudies liked this · 6 years ago
orangeblossomstudies liked this · 6 years ago -
 firmbread liked this · 6 years ago
firmbread liked this · 6 years ago -
 biopsychs reblogged this · 6 years ago
biopsychs reblogged this · 6 years ago -
 thecanadianwriter liked this · 6 years ago
thecanadianwriter liked this · 6 years ago -
 books-tea-pharmacy-blog liked this · 6 years ago
books-tea-pharmacy-blog liked this · 6 years ago -
 straightouttabakerstreet liked this · 6 years ago
straightouttabakerstreet liked this · 6 years ago -
 twohunnidtwentytwo liked this · 6 years ago
twohunnidtwentytwo liked this · 6 years ago -
 mooncakebby liked this · 6 years ago
mooncakebby liked this · 6 years ago -
 vod-kalips liked this · 6 years ago
vod-kalips liked this · 6 years ago -
 coishere reblogged this · 6 years ago
coishere reblogged this · 6 years ago